According to the National Institute of Dental and Craniofacial Research (NIDCR), temporomandibular joint disorders (TMJ), also referred to as temporomandibular disorders (TMD), are the most common source of chronic facial pain and jaw dysfunction. It is estimated that more than 10 million people in the United States are affected by temporomandibular joint problems.
What is the Temporomandibular Joint?
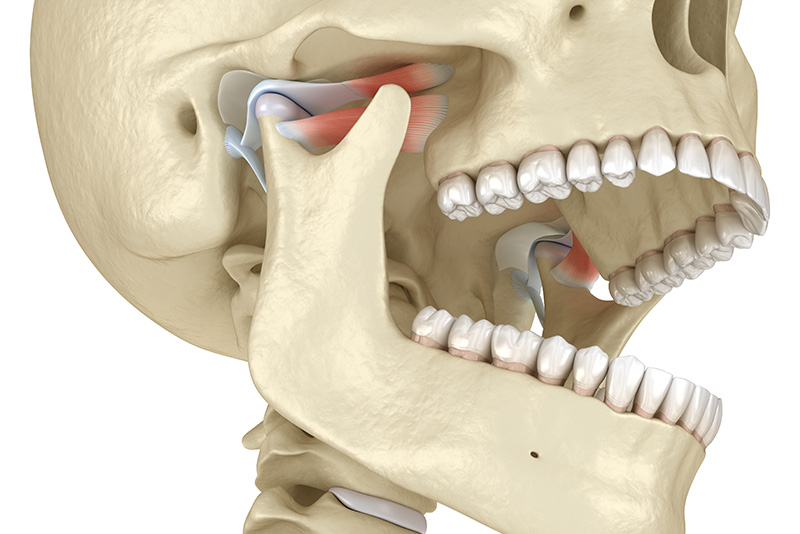
There are two temporomandibular joints that connect the left and right sides of the lower jaw to the temporal bone. Both joints and their associated muscles, ligaments and tendons work together to allow for all manner of oral function as the jaw moves up and down, front to back and from side to side. Containing a shock-absorbing, soft disc that sits between the rounded condyles of both sides of the lower jaw and the corresponding concavities in the skull’s temporal bone, the TMJ makes chewing, speaking, yawning and all jaw movements possible.
Since the TMJ is a joint with both up and down hinge-like movements, as well as side to side and front to back sliding motions to perform, it is often considered one of the most complicated joints in the body and one of the most difficult to treat when problems arise.

TMJ disorders can fall into one or more of the following three categories:
The risk for developing a TMJ problem is greater in the presence of long-term teeth grinding or bruxism, a jaw injury or various types of arthritis such as rheumatoid arthritis and osteoarthritis. Furthermore, the manifestations of a TMJ disorder can vary from person to person with a wide range of symptoms possible, including earaches, ringing in the ears (tinnitus), headaches, back and neck pain, vertigo, muscle spasms and joint tenderness as well as jaw pain, popping or grating sounds with jaw movement, jaw locking and limited jaw movement. For some people a TMJ disorder can be resolved within a relatively short period of time, while for others it will continue to persist despite extensive therapy.
Diagnosis and Treatment
When evaluating for the presence of a TMJ disorder, the dentist will perform a thorough clinical assessment of joint symptoms and function. Special radiographic imaging and other diagnostic tests will be ordered as needed. The treatment of a TMJ disorder may include oral appliances such as night guards or stabilization splints to alleviate strain on the joints. Other types of therapy may include steroid injections, occlusal adjustments as well as orthodontic or prosthodontic treatment to improve occlusion. In cases of persistent and serious TMJ problems, surgery may be recommended.
Methods of self-care can be helpful in alleviating some of the symptoms of a TMJ disorder. Patients are typically advised to eat soft foods, avoid extreme jaw movement such as wide yawning and gum chewing, to practice stress reduction and relaxation techniques and applying ice packs or moist heat as directed. If recommended, a patient should follow the dentist or therapist’s instruction for gentle stretching exercises. The short-term use of over-the-counter, non-steroidal, anti-inflammatory drugs and pain medications may provide relief. If not the dentist or physician may prescribe stronger pain or anti-inflammatory drugs, muscle relaxants or anti-depressants.
TMJ disorder refers to a group of conditions that cause dysfunction and pain in the temporomandibular joint, which connects the jawbone to the skull. It can affect jaw movement and cause discomfort.
Common symptoms of TMJ disorder include jaw pain, difficulty chewing, clicking or popping sounds when opening or closing the mouth, headaches, and earaches. Some people may also experience facial swelling and limited jaw movement.
TMJ disorder can result from various factors, including jaw injury, arthritis, teeth grinding (bruxism), misalignment of the jaw or teeth, and stress. Identifying the underlying cause is essential for effective treatment.
A dentist or healthcare professional typically diagnoses TMJ disorder through a comprehensive examination, which may include a review of your medical history, a physical examination of the jaw, and imaging tests like X-rays or MRIs if needed.
Treatment for TMJ disorder varies based on severity and may include lifestyle changes, physical therapy, medications for pain relief, dental splints or night guards, and, in some cases, surgical interventions.
Yes, stress can play a significant role in the development and exacerbation of TMJ disorder. Stress often leads to teeth grinding and clenching, which can increase tension in the jaw muscles and aggravate symptoms.
TMJ disorder is relatively common, affecting a significant portion of the population at some point in their lives. However, not everyone with TMJ symptoms will require treatment.
If left untreated, TMJ disorder may contribute to chronic pain and discomfort, affecting overall quality of life. In some cases, it can also lead to additional dental problems, such as worn teeth or jaw misalignment.
Home management techniques for TMJ disorder include applying heat or cold packs to the affected area, practicing relaxation techniques, avoiding hard foods, and performing gentle jaw exercises. Consult your dentist for personalized recommendations.
If you experience persistent pain, discomfort, or limited jaw movement, it’s essential to seek professional help. Early diagnosis and treatment can prevent the condition from worsening and improve your overall quality of life.